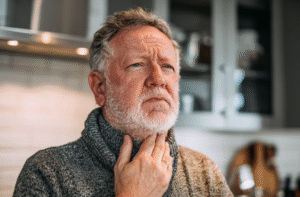
When a loved one begins showing signs of swallowing difficulties, understanding the diseases that cause dysphagia becomes crucial for providing effective care.
Recognizing which diseases that cause dysphagia your loved one may be experiencing helps you understand what to expect during their recovery journey. Some conditions offer hope for improvement, while others require long-term management strategies.
Today in this article, we will break down the most common diseases that cause dysphagia, explaining why these conditions affect swallowing function and how to recognize early warning signs in someone who is ill.
Common Diseases That Cause Dysphagia
Understanding the specific conditions behind swallowing difficulties helps families prepare for the journey ahead and make informed care decisions. The following five conditions represent the most frequent causes of dysphagia, each with distinct characteristics, recovery patterns, and care requirements.
1. Stroke
Stroke disrupts swallowing function by damaging brain areas responsible for coordinating the complex swallowing process.
According to Martino et al. (2005), stroke affects the corticobulbar pathways that control pharyngeal and laryngeal muscles essential for safe swallowing. The research found that both cortical and subcortical strokes can impair the precise timing and coordination required for the oral, pharyngeal, and esophageal phases of swallowing.
More than 50% of stroke survivors experience swallowing difficulties, though most recover within a week. For many patients, dysphagia proves temporary, with significant improvement occurring within the first few months. However, some may experience lasting difficulties requiring long-term dietary modifications. Recovery varies greatly, some regain normal swallowing within days, while others need months of therapy or permanent texture changes.
2. Parkinson’s Disease
Parkinson’s disease affects swallowing through multiple mechanisms involving dopamine depletion in the basal ganglia.
Leonard et al. (2021) explain that reduced dopamine levels impair the automatic aspects of swallowing, including reduced tongue pressure, delayed swallow initiation, and decreased laryngeal elevation. The study shows that bradykinesia (slowness of movement) and rigidity characteristic of Parkinson’s directly impact the muscles involved in chewing, tongue movement, and throat coordination.
Among progressive conditions, Parkinson’s affects muscle control throughout the body, including throat and esophageal muscles. This condition develops gradually at any disease stage, causing permanent changes that worsen over time.
While symptoms can be managed with medications, therapy, and dietary modifications, families must prepare for ongoing adaptations as the condition progresses over years rather than weeks or months.
3. Cancer
Cancer is one of the common diseases that cause dysphagia or difficulty swallowing, especially if the disease is pharynx or throat-related. Gomes et al. (2015) demonstrate that head and neck cancers can physically obstruct swallowing pathways, while radiation therapy causes inflammation, fibrosis, and reduced muscle function in treated areas. Cancer-related dysphagia results from tumors in the head, neck, or esophageal area, or from treatments like radiation and chemotherapy causing inflammation and tissue changes.
Dysphagia recovery on cancer patients depends heavily on cancer type, stage, and treatment approach. Some patients experience temporary swallowing difficulties during active treatment that resolve within months after completion, while others face permanent changes requiring ongoing dietary modifications.
4. Dementia
Dementia impairs swallowing through progressive deterioration of cognitive and motor control centers in the brain. Ward et al. (2012) explain that dementia affects the complex neural networks required for swallowing coordination, including memory for eating behaviors, recognition of food, and the ability to sequence swallowing movements.
As dementia progresses, it affects the brain’s ability to coordinate swallowing processes. This typically occurs in moderate to advanced stages, representing a permanent condition that gradually worsens over time. Unlike stroke or cancer treatment, dementia-related dysphagia doesn’t improve and requires increasingly careful management as cognitive function declines. Families need to prepare for progressive dietary changes over months to years.
5. Age-Related Changes
Among the most common diseases that cause dysphagia is the “old” disease. Age-related dysphagia results from multiple physiological changes affecting swallowing function. Rangira et al. (2022) mentioned that normal aging causes reduced muscle mass and strength in swallowing muscles, decreased saliva production, and slower neural processing.
Age-related dysphagia develops gradually and sometimes improves through exercises, medication adjustments, or treatment of underlying conditions like acid reflux. Recovery potential varies widely, some older adults see improvement with targeted interventions, while others require permanent dietary modifications.
How to Notice Dysphagia Signs in Someone Who Is Sick
Recognizing early dysphagia symptoms requires careful observation of eating and drinking behaviors. Recognizing these symptoms early can prevent complications like aspiration pneumonia and allows you to seek medical help before it’s too late.
Obvious Signs of Dysphagia:
- Coughing or choking during meals (indicates food or liquid entering the airway)
- Taking unusually long to finish meals
- Struggling with chewing and moving food around the mouth
- Drooling excessively
- Multiple attempts to swallow one bite
Subtle Signs:
- Voice changes. It can seem wet, gurgly quality after swallowing (suggests liquid pooling in the throat)
- Frequent throat clearing, especially during or after eating
- Avoiding certain textures or food types
- Eating smaller portions than usual
- Showing anxiety around mealtimes
- Holding food in the mouth without swallowing
Physical Symptoms:
- Unexplained weight loss
- Recurring respiratory infections
- Complaints of food feeling “stuck” in the throat
- Sensation that food goes “down the wrong way”
Understanding which diseases that cause dysphagia your loved one faces helps you provide better care and set realistic expectations. Each condition requires different approaches, but early recognition of symptoms and proper medical guidance make the journey more manageable. We have a helpful guide to take care of someone with dysphagia at home you can read more here.
Ready to learn more about managing dysphagia at home? Stay tuned with DysphagiaLiving.com for comprehensive guides and practical tips to live your best life with dysphagia.
References
- Cichero, J. A., Lam, P., Steele, C. M., Hanson, B., Chen, J., Dantas, R. O., … & Stanschus, S. (2017). Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: The IDDSI framework. Dysphagia, 32(2), 293-314. https://link.springer.com/article/10.1007/s00455-016-9758-y
- Leonard, R. J., Ayala, G., Sánchez, E., Alcala, J., & García, J. (2021). Thickened liquids using pureed foods for children with dysphagia: IDDSI and rheology measurements. Dysphagia, 36(5), 851-862. https://pubmed.ncbi.nlm.nih.gov/33954811/
- Martino, R., Foley, N., Bhogal, S., Diamant, N., Speechley, M., & Teasell, R. (2005). Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke, 36(12), 2756-2763. https://pubmed.ncbi.nlm.nih.gov/16269630/
- Rangira, G. D., McKinstry, C. A., Francis-Coad, J., Mulhern, B., Mnatzaganian, G., & Ratcliffe, J. (2022). The perceptions and experiences of caregivers of patients with dysphagia: A qualitative meta‐synthesis. International Journal of Nursing Studies, 136, 104357. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11366769/
- Ward, E. C., Sharma, S., Burns, C., Theodoros, D., & Russell, T. (2012). Validity of conducting clinical dysphagia assessments for patients with normal to mild cognitive impairment via telerehabilitation. Dysphagia, 27(4), 460-472. https://pubmed.ncbi.nlm.nih.gov/22407248/
- Gomes, M. d. C. M. F., Ferreira, P. M. d. V., Almeida, A. C. S. M., Cornélio, J. S., Arruda, T. J., Mafra, A., … Rezende, B. A. (2025). Dysphagia, nutritional status, and quality of life in patients with head and neck cancer undergoing radiotherapy alone or combined with chemotherapy: an observational study. BMC Cancer, 25, Article 416. https://doi.org/10.1186/s12885-025-13695‑y